Health Insurance and Autism Series. | ||
Self-funded health insurance means that your employer pays for the healthcare costs of its employees. At the beginning of every year, the employer will estimate all its employees’ healthcare costs and will ask that each covered employee pays a certain premium amount each month based on that estimate. Sometimes the employer will involve an insurance company as a “third-party administrator” to process claims and issue payments. However, the funds that pay for the costs come directly from the employer’s funds.
Self-funded plans are not subject to the same state laws as fully insured plans. As a result, they are not required to cover ABA therapy for individuals with autism. Nevertheless, there is still hope for families who have self-funded plans:
- Many employers voluntarily include ABA therapy coverage in their self-funded insurance plans,
- Even plans that do not offer ABA therapy must follow certain federal laws on how their coverage is structured, and
- Beneficiaries like you can still work with your company, coworkers, HR department, and benefits advisor to expand your plan’s coverage of ABA in future years.
Your Self-Funded Plan Might Cover ABA Therapy
More than 60% of self-funded insurance plans that cover New Jersey residents cover ABA therapy. One way to find out whether your plan covers ABA is to review the Summary of Benefits and Coverage (SBC). An SBC is a concise and easy-to-understand breakdown of the benefits of a health plan and should be given to you during the open enrollment period. If you lost your copy of your SBC, you can ask your HR representative for another.
If your SBC does not explicitly state whether your plan covers ABA therapy, that information may be in your full plan document. Employers offering self-funded health plans must still create a plan document (or use a template provided by their third-party administrator (TPA)). It will either be a single document that comprehensively lists the benefits of the plans or a template with a “wrap” document that lists coverage areas that are specifically excluded.
Read through your plan! By law, the language around plan benefits should be clear and unambiguous. When it’s not clear, some families have been successful in getting their plan to cover ABA when that treatment was not specifically excluded. Either way, beneficiaries can still appeal improper coverage denials. If your plan does not cover ABA therapy, see the section below, titled “Advocating for Increased Coverage.”
Legal Requirements for Self-Funded Plans
While self-funded plans are not subject to certain state laws, such as the Autism Insurance Mandate, federal law still states that your plan must offer mental and behavioral health in parity with any medical or surgical benefits it offers. This means that your health insurance plans can’t apply a limitation on its coverage of outpatient behavioral health benefits (such as Applied Behavior Analysis therapy) if the same limitation is not applied to substantially all coverage for outpatient medical or surgical benefits. The federal law that guarantees parity is the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA).
Examples of MHPAEA Violations
The following policies are examples that, whether explicitly written into a plan or carried out in practice, would violate MHPAEA’s parity requirement
- Your employer or their TPA puts a dollar cap on coverage of medically necessary ABA when no such dollar cap exists for physical therapy due to a back injury
- Your employer or their TPA requires a parent to be present or to participate during ABA therapy sessions but would not require the same parent participation for a child during their chemotherapy sessions
- Your employer or their TPA states that a beneficiary is only covered for a maximum of 100 hours of ABA per
Advocating For Increased Coverage
If your self-funded plan does not cover ABA therapy, there’s still hope! There are several strategies you can employ to work towards coverage of ABA therapy your child might get in the future.
Talk to your employer to see if your benefits administrator can expand the employee plan next year to include ABA therapy. The coverage details of a self-funded plan – including premium cost and what treatments are covered – are set by the employer. As a result, you may be able to make a convincing case for them to include coverage of ABA therapy in subsequent years.
You may enlist the help of your coworkers as well. New Jersey has one of the highest rates of autism in the nation. There is a good chance that someone you work with has a child or family member with autism, too. More people making the same request might give you additional bargaining power when communicating with your employer.
You may be successful in convincing your employer that, while the incremental costs of including ABA coverage in a self-insured health plan are often as low as increasing the price of the premium for each member by $1 per month, the costs a single family without coverage may incur can be financially devastating.
For more information and resources, check out our page on Treatment, our own Autism New Jersey ABA fact sheet, and the Autism Speaks Self-Funded Employer Toolkit.
If your employer’s plan doesn’t cover ABA, here are other options to explore:
- Look into financial assistance options: While you work to get ABA covered in subsequent plan years, you can seek assistance from the Catastrophic Illness in Children Relief Fund. )The Fund – provides financial help for New Jersey families overwhelmed by a child’s medical bills. They reimburse families that spend 10% of their income (as well as 15% of any income over $100,000) on a child’s medical bills during a 12-month period, so long as those expenses are not covered by insurance. Those bills can include payment for ABA therapy.
- Purchase a Child-Only Plan: You can also try to buy a fully insured child-only plan through the New Jersey State health insurance marketplace. For information on how to purchase a child only plan, see our article, Child-Only Health Insurance Plans >>
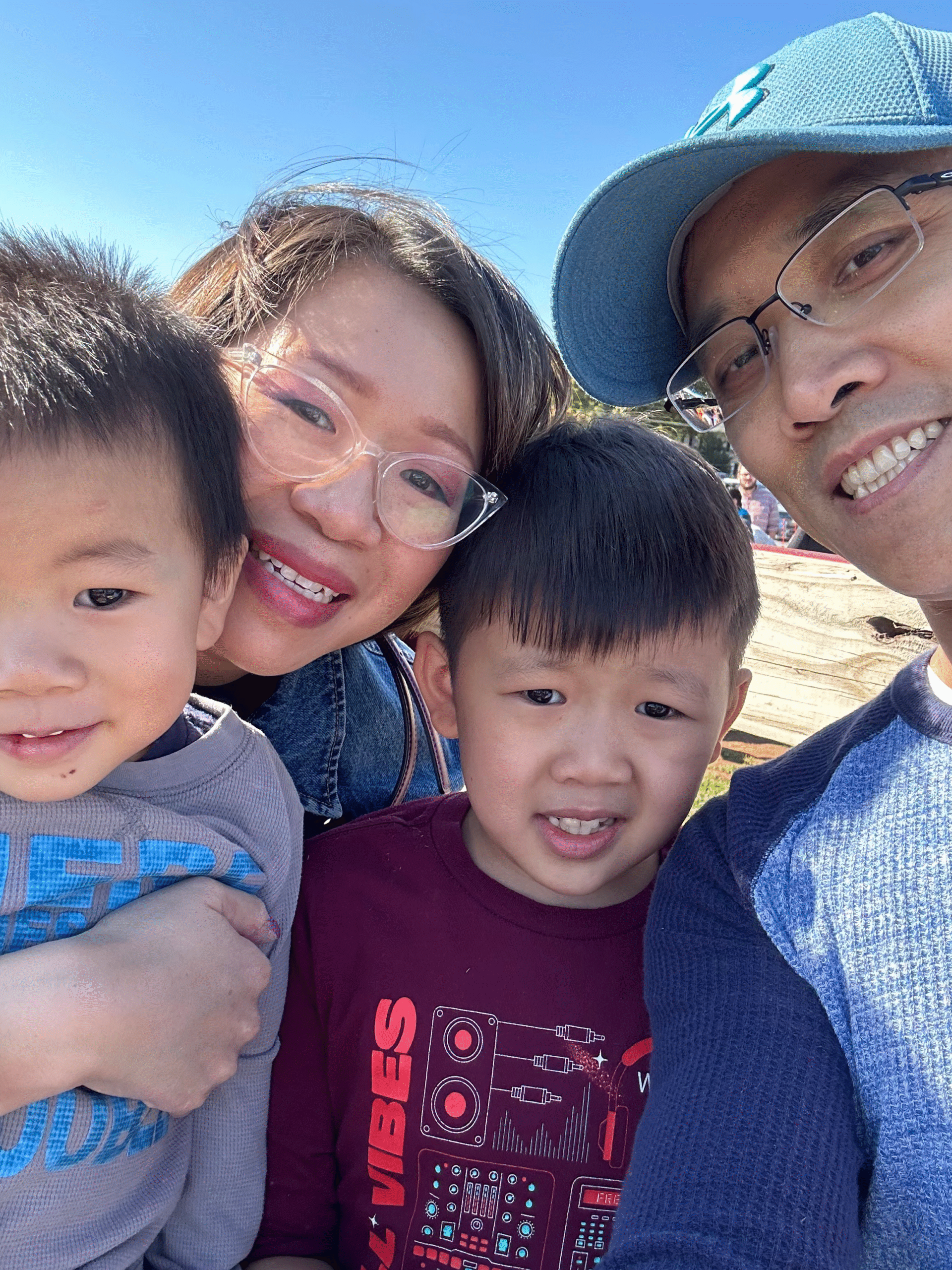
Need Help?
If you can’t figure out what type of health insurance you have, or if you have other questions about insurance and how to use it to cover autism diagnostic evaluations or applied behavior analysis, visit our insurance hub>>
Connect with an Autism New Jersey Helpline Specialists. Call 800.4.AUTISM Helpline or email information@autismnj.org.