General Considerations for Pediatricians
It is common practice for a pediatrician to refer a patient to a developmental behavioral pediatrician when there are developmental concerns specific to a potential autism diagnosis. In some situations, this is clinically appropriate.
Pediatricians should likely continue this practice of referral for patients who:
- Are older than 4 years old
- Have signs and symptoms that are not clearly signs of autism and other diagnoses should be ruled out first
- Have family or guardians who do not seem likely or ready to accept the diagnosis
Pediatricians should consider providing an autism diagnosis for patients who:
- Are between 18 months and 4-years-old
- Showing very clear signs and symptoms of autism and/or score as high-risk on the M-CHAT- R/F
- Have family or guardians who are aware of these concerns and seem ready to accept the diagnosis
The American Academy of Pediatrics provides an excellent resource for pediatricians considering providing autism diagnoses in their primary care practice.
Autism Diagnosis in Primary Care
Diagnostic Criteria for Autism Spectrum Disorder
To accurately and effectively diagnose autism, it is essential to become knowledgeable about the diagnostic criteria.
The American Psychiatric Association (APA) Diagnostic and Statistical Manual of Mental Disorders (DSM) is the resource used by health care professionals to guide them in diagnosing Autism Spectrum Disorder.
To be diagnosed with Autism Spectrum Disorder (ASD), your patient must meet a specific number of criteria from two major categories: deficits and difficulties with social communication and interaction and restricted, repetitive patterns of behavior, interests, or activities.
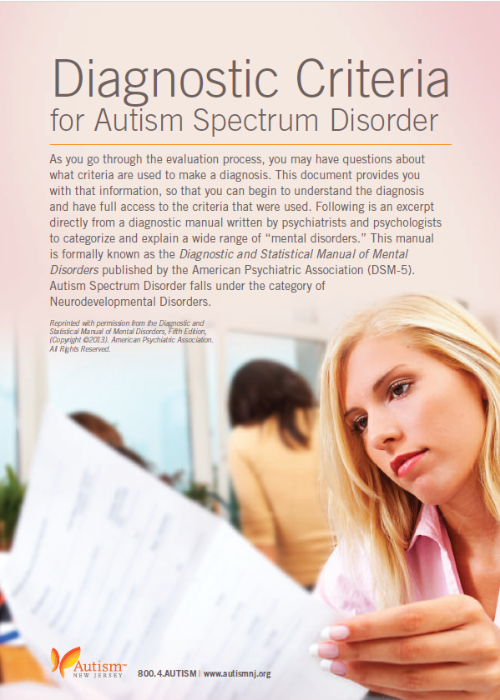
It is important to note that these levels are only related to the autism diagnosis. While it is likely that someone with a co-occurring intellectual disability needs a higher level of support, that does not necessarily mean they have Level 3 Autism. Intellectual disability, while co-occurring in a little more than one-third of those with autism, is a distinct diagnosis and may not impact the level of autism severity.
View the full diagnostic criteria for Autism Spectrum Disorder
Use of Formal Diagnostic Assessments
While not required for a valid diagnosis, most clinicians support an autism diagnosis based on parent report and direct observations with a formal diagnostic assessment. In addition to supporting their clinical judgment, formal assessments are often required by insurance companies.
The assessment most frequently referenced is the Autism Diagnostic Observation Schedule, 2nd Edition (ADOS-2), and is often seen as the “gold standard.” Pediatricians are able to attend training on the use of this assessment.
A.J. Drexel Autism Institute and CHOP ADOS-2 Training
A drawback to the ADOS-2 is the lengthy training become a competent assessor, and more importantly, the time required to utilize it with a patient. Many pediatricians may not have 1-2 hours to spend with a patient. The good news is that research supports that a skilled diagnostician does not need to use the ADOS-2 in all cases, and most developmental behavioral pediatricians agree with that finding. Also, there are other valid assessment tools.
Below are several other formal assessments that pediatricians can consider using instead of the ADOS-2:
Autism Diagnostic Interview-Revised (ADI-R)
Childhood Autism Rating Scale, 2nd Edition (CARS-2)
Gilliam Autism Rating Scale, 3rd Edition (GARS-3)
Screening Tool for Autism in Toddlers and Young Children (STAT)
Rapid Interactive Screening Test for Autism in Toddlers (RITA-T)
Formal Documentation of an Autism Diagnosis
Clear documentation of a medical diagnosis of autism is required to be eligible for some autism services, including Applied Behavior Analysis (ABA) covered by insurance.
Diagnostic reports should include the following important components:
- A clearly documented Autism Spectrum Disorder diagnosis, including the severity level (do not use phrases such as “history of” or “rule out” unless that is what is truly appropriate)
- A direct reference to the DSM-5 diagnostic criteria
- A summary of parent report and direct observations
- Results of any formal diagnostic assessments
- A statement that it is a differential diagnosis
In addition, the diagnosing clinician may also write a prescription for ABA. This prescription should include the following:
- Patient information (DOB, history, etc.)
- Diagnosing provider’s information
- Clear statement of the autism diagnosis
- Clinical and functional presentation of the diagnosis for the patient
- A statement that the prescription is to evaluate and treat
- A statement that the treatment is medically necessary
- Recommended intensity of services (number of weekly hours)
- Inclusion of parent training
The New Jersey Department of Health Autism Registry
The New Jersey Department of Health created an autism registry in 2007 to better understand autism in the state and link families and children to special child health case management services. The diagnosing provider is responsible for adding the patient to the registry.
NJ Department of Health Autism Registry
Families may opt to have their child added to the registry anonymously (which is fine but it will not link them to services), and they may have additional questions.