The Road to Medicaid Coverage of ABA
June 14, 2020
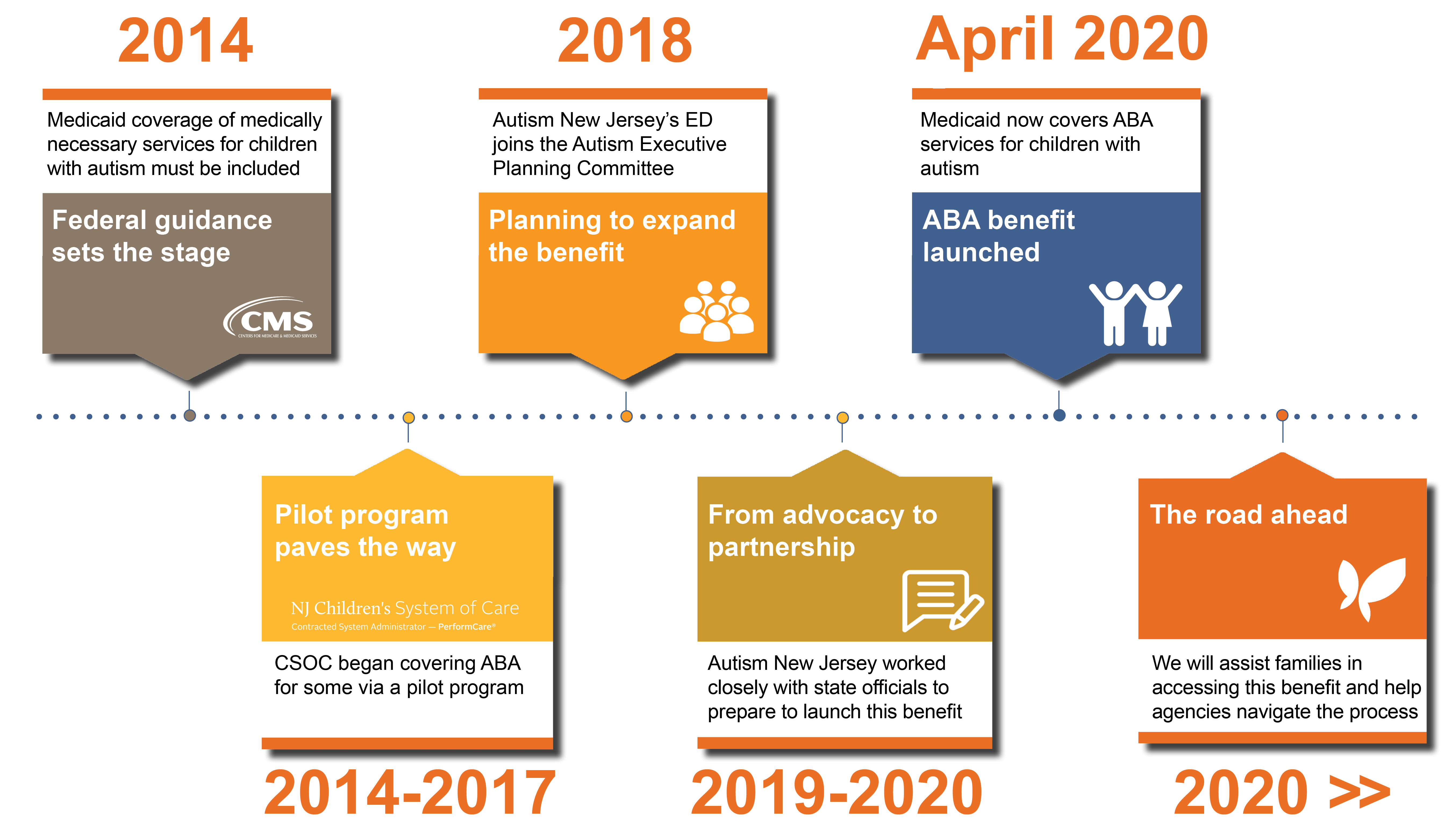
Amidst and possibly overshadowed by the COVID-19 pandemic, the state Medicaid program, NJ FamilyCare, launched the long-anticipated ABA benefit on April 1, 2020. Medicaid — health coverage that brings medically-necessary treatment to 40% of all New Jersey children — now covers Applied Behavior Analysis (ABA) services for children with autism. We repeat: Medicaid covers ABA. Finally.
For those in the know, that’s very big news. It opens the door to coverage to thousands of low-income children previously unable to access autism treatment. If you’re wondering to yourself, “I thought there was an Insurance Mandate that covered that already,” the answer is “no.” That hard-fought legislation passed in 2009 covered only some types of private insurance. The path to Medicaid – a publicly-funded federal program administered by states — is another story.
Medicaid is a huge program that covers 63.9 million Americans and is fraught with requirements and regulations. Autism New Jersey’s dogged determination to untangle these regulations, combined with its public policy and technical expertise, were essential on the long road to Medicaid coverage of ABA.
 Federal guidance sets the stage (2014)
Federal guidance sets the stage (2014)
On July 7, 2014, five years after the private autism insurance mandate passed, the Centers for Medicare & Medicaid Services (CMS) issued an informational bulletin clarifying that Medicaid coverage of medically necessary services for children with autism must be included in a state’s Medicaid plan under its EPSDT program.* It gave states the authority to decide how to implement the guidance, requiring them to submit a State Plan Amendment or SPA outlining their plans.
Consistently for the last six years and spanning two administrations, Autism New Jersey has worked closely with the two state agencies tasked with its implementation of this benefit — the Department of Children and Families (DCF) Children’s System of Care (CSOC) and the Department of Human Services (DHS) Division of Medical Assistance and Health Services (DMAHS) — to ensure that it stayed at the forefront of their agenda.
 Pilot program paves the way (2014-2017)
Pilot program paves the way (2014-2017)
Shortly after CMS released its guidance, CSOC began covering Applied Behavior Analysis (ABA) services for some Medicaid-eligible children via a pilot program under the New Jersey Comprehensive Waiver. The scope of this pilot was limited to only a few hundred children and the acuity threshold to access this service was high, meaning that children had to exhibit severe challenging behavior to qualify. Nevertheless, it was a step in the right direction.
Autism New Jersey partnered with CSOC and its contracted system administrator, PerformCare, to provide ongoing technical assistance and policy recommendations. Autism New Jersey, CSOC, and PerformCare collaboratively developed quality assurance measures, provided collegial feedback on treatment plans to providers and care managers, and addressed systemic trends.
With the pilot program set to expire on June 30, 2017, and an expectation of a federal requirement to expand this benefit to all Medicaid-eligible children on the next day, our efforts during this time were focused on building a robust and accountable service delivery system to prepare for the expansion.
 Planning to expand the benefit (2018)
Planning to expand the benefit (2018)
In the summer of 2018, Autism New Jersey’s Executive Director, Dr. Suzanne Buchanan, was invited by DMAHS and CSOC to participate in their newly formed Autism Executive Planning Committee that would provide expert recommendations on the design of this benefit. As a member of the committee, Dr. Buchanan was an assertive proponent of easy access for families and evidence-based treatments. Dr. Buchanan’s extensive knowledge of how other states have implemented this benefit and her experience in leading the advocacy efforts of the Autism Insurance Mandate in 2009 proved invaluable and helped shape the path of this benefit.
 From advocacy to partnership (2019-2020)
From advocacy to partnership (2019-2020)
Throughout 2019, Autism New Jersey continued to lead the advocacy efforts for this benefit while working closely with DMAHS and CSOC. In January, we provided public comment at the Division’s open forum and submitted written testimony while garnering the support of approximately 100 other professionals and parents to do the same.
Over the course of the year, we had several meetings with the DHS and DCF commissioners and their staff to share families’ urgency to access this benefit, offer administrative recommendations (e.g., how the benefit should be administered, disallowing any improper limitations to coverage), introduced them to two attorneys with national expertise in the matter, and had frequent meetings and phone calls with DMAHS as they finalized the details of this benefit.
 The road ahead
The road ahead
With the benefit now live and accessible to families, we are pleased to see that our years of persistence and scientifically-informed advocacy will now begin to pay dividends to the those families that need it the most. Although it has been a long road to get to this point, we realize our work is not done. We will be here to assist families in accessing this benefit and ensuring they get the services that they need, help agencies navigate the process of becoming Medicaid providers, and continue to work closely with DMAHS to provide assistance and feedback.
Experience Our Power of Connection
Need assistance understanding Medicaid/NJ Family Care? Contact our 800.4.AUTISM Helpline. Since we are working remotely, please leave a message with specific dates and times you are available for a call-back, or email information@autismnj.org. You can also chat or message us via our website link and we’ll aim to reply promptly.
Membership dues help sustain Autism New Jersey’s public policy work. Please consider joining as a member or making a donation so we can continue advocating for important issues like this one!
*Note: The justification for this coverage fell under Medicaid’s EPSDT’s program, which has been in place for decades. The Early and Periodic Screening, Diagnostic and Treatment (EPSDT) benefit provides comprehensive and preventive health care services for children under age 21 who are enrolled in Medicaid. EPSDT is key to ensuring that children and adolescents receive appropriate preventive, dental, mental health, and developmental, and specialty services.

 Federal guidance sets the stage (2014)
Federal guidance sets the stage (2014) Pilot program paves the way (2014-2017)
Pilot program paves the way (2014-2017) Planning to expand the benefit (2018)
Planning to expand the benefit (2018) From advocacy to partnership (2019-2020)
From advocacy to partnership (2019-2020) The road ahead
The road ahead