On January 16, 2024, Governor Murphy signed the “Ensuring Transparency in Prior Authorization Act,” P.L. 2023, c. 296 (A1255/S1794). The law’s proponents sought to clarify and streamline the insurance claim process for prior authorizations and make sure that, when insurance claims are approved or denied, the reviewer at the insurance company has the proper expertise.
This process makes sense in a medical context. If someone has a cancer diagnosis that requires chemotherapy, it follows that only a physician with an expertise in cancer treatment should be able to deny treatment that an oncologist prescribes. The law would prevent someone with different credentials, like a nurse practitioner, or another type of doctor, like a podiatrist, from pushing back on treatment prescribed by a specialist.
However, there may be issues if you apply this idea to ABA therapy without adapting it to better fit the ABA healthcare model. Under the language of the statute, only a physician with experience in the treatment can approve a prior authorization request or review an appeal. However, Board Certified Behavior Analysts (BCBAs), not physicians, are the treating healthcare professionals for ABA therapy
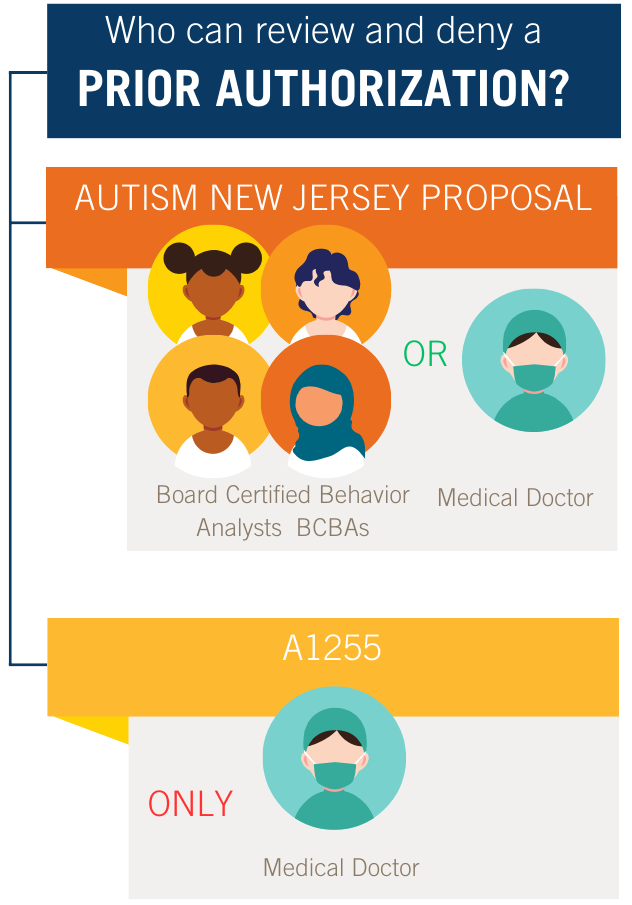
If applied exactly as written, the law gives insurance companies no leeway. They won’t have enough staff who can legally and efficiently review prior authorization claims for ABA therapy.
As the bill advanced through the legislative process, Autism New Jersey advocated for amendments to ensure that ABA therapy would not be an unintended casualty of this bill. We asserted that prior authorization requests should be allowed to be evaluated by those most familiar with the science and research that guides ABA treatment. We testified before legislative committees, provided written advocacy submissions to the Legislature and the Governor, and met with other stakeholder groups engaged in this legislation.
That said, the procedural history of this bill was complex. It was amended several times and required considerable negotiations between those supporting the interests of the medical field and those of the insurance companies. Because of these drawn-out, multilayered negotiations and the legislative fatigue of those involved, we did not achieve our goal. The language regarding the prior authorization review process went to the Governor’s desk unchanged.
Despite the exclusion of our requested amendments, our advocacy continues in the form of monitoring implementation. We are keeping an eye on how this law will play out for the autism community. If this law has the unintended effect of limiting access to treatment for people with autism, it can and should be amended.
We remain dedicated to individuals with autism, their families, and the treatment providers who serve them. We will continue to watch this issue and work to bring to light any of the collateral negative consequences that this law might have on the autism community. Please reach out to our 800.4.AUTISM Helpline if you are a parent or an autism treatment provider currently having trouble navigating a prior authorization review for autism treatment services.